Hypothalamic Amenorrhea recovery signs can be something to really look out for in eating disorder recovery as they show that your body is healing. Losing a period is something that I come across a lot in my clinical work and I don’t think it is talked about enough. When we talk about women’s health, you might not hear the word “amenorrhea” every day, but it’s crucial to be aware of it, especially if you have a uterus.
If you have disordered eating, a restrictive eating disorder, if you exercise to a high level or have gone through a highly stressful period of time then this could apply to you. In this blog we will break down what amenorrhea is, focusing on a specific type called Functional Hypothalamic Amenorrhea (FHA). We’ll explore the causes, symptoms, consequences, and how it can be diagnosed and treated. Then we will look at those all important hypothalamic amenorrhea recovery signs too.

What is amenorrhea?
Amenorrhea is a medical term meaning the absence of periods or menstruation (1). While it’s normal during pregnancy, breastfeeding, or before and after menopause, having amenorrhea outside of these situations might indicate an underlying issue.
There are two main types:
- Primary Amenorrhea – when a woman does not starts her period in the first place. Primary amenorrhea is usually due to genetic or anatomical reasons and should be investigated if your period has not started by age 16yrs (1).
- Secondary Amenorrhea – when someone had regular periods but they stop for more than 3 months or become irregular for over 6 months (2). It is normal for women to miss a period from time to time, it’s only when it is missed for several consecutive months that it may be amenorrhea.
Note: Amenorrhoea is different from oligomenorrhea, which is the medical term for ‘irregular periods’. Oligomenorrhoea occurs when the gaps between periods keep changing unpredictably which can happen throughout a women’s life cycle (3).
Menstruation: The Basics:
To help you fully understand Functional Hypothalmic Amenorrhea let’s take a brief look at the physiology behind menstruation.
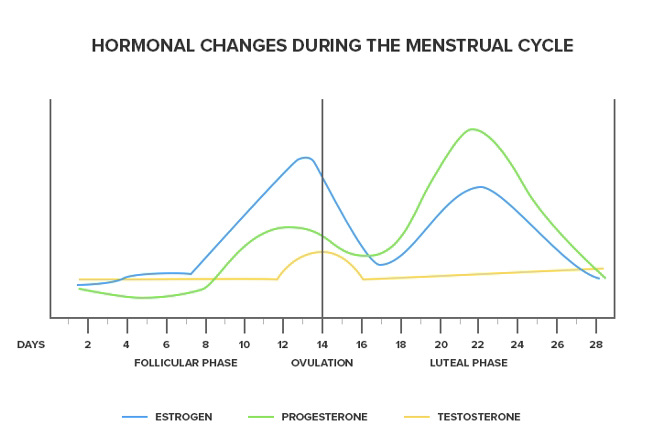
Menstruation describes the female period. Each month women’s body’s prepare for them to become pregnant. A complex system of hormones released from the brain controls the menstrual cycle (4). Each month rising levels of the hormone oestrogen cause the ovary to develop and release an egg (ovulation) (4) . Alongside rising levels of oestrogen, progesterone levels also increase causing the endometrium lining of the uterus to become thicker and softer creating a perfect environment for an egg to implant (4). If an egg does not implant and isn’t fertilised, the thicker endometrium layer sheds and we get the bleeding we know as a period. The cycle then begins again and the process repeats itself each month. The average cycle length of a period is 28 days with 5 days of bleeding (4),(5).
What is functional hypothalamic amenorrhea?
Functional Hypothalamic Amenorrhea (FHA) is a specific type of amenorrhea linked to dysfunction in the hypothalamus, a crucial part of the brain that regulates various bodily functions, including the menstrual cycle (3). It happens when the hypothalamus slows or stops producing certain reproductive hormones (6).
The science bit:
The hypothalamus is found at the base of the brain and plays an important role in releasing reproductive hormones. It produces a hormone known as gonadotropin-releasing hormone (GnRH). GnRH signals the production of other hormones needed for egg maturation and ovulation, such as follicle-stimulating hormone (FSH), luteinising hormone (LH) and oestrogen (4). Sometimes the hypothalamus does not produce sufficient amounts of GnRH which can in turn reduce the amount of other reproductive hormones (FHA, LH and oestrogen) produced. This has a knock-on effect that can stop ovulation and menstruation (4).
Causes of functional hypothalamic amenorrhea
The causes of FHA are mainly related to psychological stress, excessive exercise, disordered eating, low body weight or a combination of the above (7). When the body is put under severe stress, it stops menstruating. This is believed to be an evolutionary response in which the body prioritises supporting other ‘more important’ aspects of physiological health rather than menstruation (7). It makes sense, the body is protecting itself and stopping some functions that use more energy.
Several factors can contribute to the development of FHA:
- Stress: High levels of physical or emotional stress can disrupt the delicate hormonal balance needed for regular menstruation.
- Weight Loss or Low Body Weight: Significant weight loss or maintaining a low body weight, often associated with intense physical training or restrictive eating, can impact hormonal signals controlling the menstrual cycle.
- Excessive Exercise: Intense or excessive exercise without adequate recovery periods can interfere with the body’s hormonal regulation.
- Psychological Factors: Mental health plays a crucial role. Conditions like anxiety, depression, or chronic stress can influence hormonal balance.
While anyone can experience FHA there are certain groups of women who are more at risk:
- Women with eating disorders or disordered eating: Some characteristics that contribute to FHA are common in women with eating disorders or disordered eating such as, calorie restriction, excessive exercise, and/or psychological stress.
- Professional athletes: Even women that are eating enough may experience FHA if they are athletes. This is because they are putting their body under high physical stress by intensely exercising. Many athletes lose their period by being in a slight, persistent energy deficit—oftentimes unknowingly. This is called Relative Energy Deficiency Syndrome or REDs for short(9).
How is functional hypothalamic amenorrhea diagnosed?
The diagnosis of FHA is a diagnosis of exclusion. This means that other conditions such as thyroid dysfunction and polycystic ovary syndrome have to be ruled out before FHA can be diagnosed. This can take time! As part of this process, your doctor might look at the following:
- Medical History: Understanding the individual’s medical history, lifestyle, and stressors.
- Physical Examination: Assessing overall health.
- Hormonal Testing: Measuring hormone levels, such as oestrogen, luteinising hormone (LH), and follicle-stimulating hormone (FSH), to identify abnormalities.
Health impacts of functional hypothalamic amenorrhea
Untreated FHA can lead to:
- Cardiovascular disease: Low oestrogen levels have been linked to early cardiovascular disease (CVD) (5). Research from the Nurses’ Health Study looked at data from over 82,000 women. It was found that the more irregular the menstrual cycle in young women the greater the risk for future cardiovascular disease events (with up to a 50% increase) (6)
- Bone health: Oestrogen plays an important role in maintaining healthy bones as well as healthy menstrual cycles. Having low oestrogen levels can increase risk of bone disease in later life. Functional Hypothalamic Amenorrhea can impacs the absorption of calcium and can pose a risk to young women for developing osteopenia or osteoporosis at an early age and/or over their lifetime (7)
- Psychological impact: Psychological stress can be a cause of FHA and also FHA can cause stress! Women with FHA have been shown to have significantly higher depression scores and greater anxiety, compared to those without FHA (8). Perfectionistic behaviour and extra attention to the judgements of others has also been found to be more common in women with FHA in comparison to those with a normal, regular menstrual cycle.
- Fertility: Unfortunately, if left untreated, FHA can impact reproductive health. Prolonged amenorrhea can make it more difficult to get pregnant. So regaining a regular cycle is so key. FHA typically occurs during peak reproductive years, resulting in anovulation (the lack or absence of the release of an egg) and infertility.
Treatment for missed periods:
Treating FHA aims to restore a regular menstrual cycle. It involves a holistic approach that addresses the underlying cause of stress is often the most effective. This may include treatment for disordered eating, stress management and/or excessive exercise. This can include:
- CBT : Cognitive behavioural therapy (CBT) has been shown to be a successful treatment option for FHA. It can help lower levels of stress through lowering cortisol levels (stress hormone) in women with FHA.
- Seeking advice from a registered dietitian : A dietitian can help you improve your energy balance and relationship with food. Advice may be centred around increasing calorie consumption, including all the food groups, rebuilding your relationship with food and your body, improving nutritional quality of the diet and/or reducing physical activity levels. Reducing exercise may also need to be part of the plan as rest is really key.
- Stress management: Mediating stress through incorporating stress management practices has been shown to help treat FHA. Stress management techniques may include yoga, journaling, sleeping sufficiently and CBT.
- The pill : While this could sound like a good option, it isn’t the answer. Oral contraceptive therapy (or the pill) is an oestrogen replacement that provides a withdrawal bleed, however it does not support the resumption of normal hormone activity. The underlying cause of FHA still needs to be addressed and this is something we would suggest you work on first. The endocrine society clinical practice guidelines suggest against women with FHA using oral contraceptive pills for the sole purpose of regaining menstruation
Note: What treatment method works for one person may not work for another. That is why it is important to seek individual advice from a healthcare professional.
Hypothalamic amenorrhea recovery signs
Recovery from FHA is important for overall health, especially bone health and fertility. Here are some key hypothalamic amenorrhea recovery signs to look out for:
Hypothalamic Amenorrhea Recovery Signs to look for:
- Improved Energy Levels: Recovery from FHA often comes with increased energy levels and a reduction in fatigue. This is because the body is no longer in a state of energy deficit, which can occur with disordered eating or excessive exercise.
- Better Mood and Mental Health: Hormonal imbalances that occur with HA can impact mood and mental health. As hormonal levels stabilise with recovery, many women can experience improvements in mood, reduced anxiety, and better overall mental well-being.
- Increase in Libido: Hormonal changes associated with recovery can lead to an increase in libido or sexual desire.
- Improved Bone Health: Oestrogen plays a critical role in maintaining bone density. Recovery from FHA can lead to improvements in bone health, reducing the risk of osteoporosis and fractures. This recovery sign could be noted on your DXA scan.
- Changes in Body Composition: With recovery, some individuals may notice changes in body composition, including an increase in body fat percentage and restoration of curves, particularly in areas like the breasts and hips. This can be a really tricky one of the hypothalamic amenorrhea recovery signs to work through. Try to keep focused on the fact that your body needs body fat to make hormones and function well.
- Improvement in Hormonal Levels: Blood tests can reveal changes in hormone levels associated with HA, such as increases in oestrogen, luteinizing hormone (LH), and follicle-stimulating hormone (FSH), indicating that the hypothalamus is once again signalling the ovaries to produce hormones.
- Return of Menstrual Cycle: The most obvious of the hypothalamic amenorrhea recovery signs is the return of regular menstrual cycles. This means having periods every 21 to 35 days, with consistent flow and duration.
Conclusion
Remember, what works for one person may not work for another. Seek individual advice and support from a healthcare professional. FHA is reversible, and with the right help, you can restore your period and bring long-term healing to your relationship with food and your body. If you’re concerned, reach out to your GP for guidance as a starting point. We are always happy to help you in the Dietitian UK clinic.
References
- National Institute for Health and Care Excellence (NICE)., 2021. https://cks.nice.org.uk/topics/amenorrhoea/
- MCCLINTOCK, A. & KAMINETZKY, C., 2020. https://link.springer.com/chapter/10.1007/978-3-030-34814-4_46
- GORDON, C. M., et al., 2017. https://academic.oup.com/jcem/article/102/5/1413/3077281
- JARRELL, J., 2018. The significance and evolution of menstruation. Best practice & research. Clinical obstetrics & gynaecology [online]. 50, pp. 18–26. [Viewed 3 July 2021]. Available from: https://pubmed.ncbi.nlm.nih.gov/29530426/
- MIHM, M., GANGOOLY, S & MUTTUKRISHNA, S., 2011. https://www.sciencedirect.com/science/article/abs/pii/S0378432010004148
- O’DONNELL, E., HARVEY, P,J ., GOODMAN, J, M ., DE SOUZA, M, JANE., 2007. https://pubmed.ncbi.nlm.nih.gov/17227959/
- SOLOMON, C. G., et al., 2013. https://pubmed.ncbi.nlm.nih.gov/11994334/
- MECZEKALSKI, B., PODFIGURNA-STOPA, A & GENAZZANI AR., 2010. https://www.tandfonline.com/doi/full/10.3109/09513590.2010.486452
- MARCUS, M. D., LOUCKS, T, L ., BERGA, S, L., 2001. https://pubmed.ncbi.nlm.nih.gov/11476778/